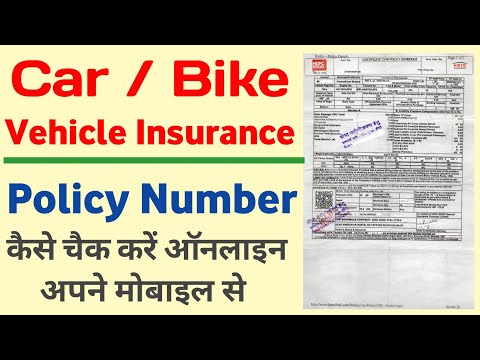
Each person covered by a health insurance plan has a unique ID number that allows healthcare providers and their staff to verify coverage and arrange payment for services. It's also the number health insurers use to look up specific members and answer questions about claims and benefits. If you're the policyholder, the last two digits in your number might be 00, while others on the policy might have numbers ending in 01, 02, etc. If you see two numbers, the first is your cost when you see an in-network provider, and the second—usually higher—is your cost when you see an out-of-network provider. For example, when you're referred to a specific specialist or sent to a specific hospital, they may not be in your insurer's network.
If you do not see your coverage amounts and co-pays on your health insurance card, call your insurance company . Ask what your coverage amounts and co-pays are, and find out if you have different amounts and co-pays for different doctors and other health care providers. Finally, you might see a dollar amount, such as $10 or $25. This is usually the amount of your co-payment, or "co-pay." A co-pay is a set amount you pay for a certain type of care or medicine. Some health insurance plans do not have co-pays, but many do. If you see several dollar amounts, they might be for different types of care, such as office visits, specialty care, urgent care, and emergency room care.
If you see 2 different amounts, you might have different co-pays for doctors in your insurance company's network and outside the network. An insurance plan that has contracts with health care providers for discounted charges. Typically, the plan offers significantly better benefits and lower costs to the patients for services received from preferred providers. A doctor, hospital, or other health care entity that is not part of an insurance plan's network. For medical services rendered by non-participating provider, the patient may be responsible for payment in full or higher costs. A group of doctors, hospitals, and other health care providers that have a contract with an insurance plan to provide services to its patients.
A member ID number and group number allow healthcare providers to verify your coverage and file insurance claims for health care services. It also helps UnitedHealthcare advocates answer questions about benefits and claims. Under M+C plans, patients receive medical services without additional out-of-pocket costs. You might see another list with 2 different percent amounts. Your insurance company may provide out-of-area coverage through a different health care provider network.
If so, the name of that network will likely be on your insurance card. This is the network you'll want to seek out if you need access to healthcare while you're away on vacation, or out of town on a business trip. Policy Number - a number that the insurance company assigns the patient to identify the contract for coverage. A doctor, hospital, or other health care entity that is part of an insurance plan's network.
They agree to accept insurance payment for covered medical services as payment in full, less any patient liability. Your member ID number and group number allow healthcare providers to verify your coverage and file claims for health care services. These numbers also help UnitedHealthcare advocates answer questions about your benefits and claims.
If you forget or aren't sure what type of health insurance plan you have , you can find out on your BCBS ID card. If you have an HMO, your card may also list the physician or group you've selected for primary care. Determining whether a provider is in-network is an important part of choosing a primary care physician.
If you have health insurance through work, your insurance card probably has a group plan number. The insurance company uses this number to identify your employer's health insurance policy. When you get a health insurance policy, that policy has a number. On your card, it is often marked "Policy ID" or "Policy #." The insurance company uses this number to keep track of your medical bills. Your health insurance company might pay for some or all the cost of prescription medicines. If so, you might see an Rx symbol on your health insurance card.
But not all cards have this symbol, even if your health insurance pays for prescriptions. Sometimes, the Rx symbol has dollar or percent amounts next to it, showing what you or your insurance company will pay for prescriptions. A private insurance plan that accepts people with Medicare.They may go to any Medicare-approved doctor or hospital that accepts the plan's payment. The insurance plan, rather than the Medicare program, decides how much it will pay and what the beneficiary will pay for the services they get.
The beneficiary may pay more for Medicare-covered benefits. They may have extra benefits the Original Medicare Plan does not cover. An alternative to the Original Medicare Plan which replaces the Original Medicare Plan and often named as Senior plans following the name of the insurance. The "coverage amount" tells you how much of your treatment costs the insurance company will pay.
This information might be on the front of your insurance card. It is usually listed by percent, such as 10 percent, 25 percent, or 50 percent. For example, if you see 4 different percent amounts, they could be for office visits, specialty care, urgent care, and emergency room care. After going through, one can get a pretty straightforward idea about the health insurance cards. I think that it is a good idea to maintain an effective health insurance coverage. I think that the cards should also link the patient's previous medical history.
When you go to an appointment with your health care provider, they will ask you for your insurance information. Groups with the BlueStagesSM will see the plan name Blue Cross Group Medicare SupplementSM on their member ID cards for 2020. This Medicare supplement insurance plan helps members cover some costs not covered by Original Medicare, such as copayments and deductibles.
Members can see providers nationwide who accept Medicare Assignment and are willing to bill BCBSTX. To find out if a provider is "in network" contact your insurance company. The descriptions below apply to most private health insurance ID cards in the United States. If you live outside the U.S. or have government-provided insurance, you may see some different fields on your card.
A group of primary care physicians who have agreed to share the risk of providing medical care to their patients who are covered by a given health plan. A description of the health care coverage included in an insurance company's plan. The certificate of coverage is required by state laws and explains the health care coverage provided under the contract issued to the employer. The back of your member ID card includes contact information for providers and pharmacists to submit claims. It also includes the member website and health plan phone number, where you can check benefits, view claims, find a doctor, ask questions and more.
Checking eligibility and benefits and/or obtaining benefit prior authorization/pre-notification or predetermination of benefits is not a guarantee that benefits will be paid. Regardless of any benefit determination, the final decision regarding any treatment or service is between you and your patient. If you have any questions, please call the number on the member's ID card. Beginning January 1, 2020, health care providers will notice new Blue Cross Medicare and Medicare Supplement group plan names and ID cards. Blue Cross Medicare AdvantageSM plan names for individuals will remain the same.
Every health insurance card should have the patient's name on it. If you have insurance through someone else, such as a parent, you might see that person's name on the card instead. The card might also include other information, such as your home address, but this depends on the insurance company. Most health insurance cards contain straightforward identification information about the people covered and the policy you have. An agreement by insurance company to pay for medical services. Physicians and hospitals ask the insurance company for this approval before providing medical services.
What Is Group Name On Anthem Insurance Card Failure to get the approval often results in a penalty to the patient since the services may not be covered by insurance. Type of medical service used by doctors and hospitals to determine whether the patient needs inpatient care, outpatient care or whether they can recover at home. Observation is usually charged by the hour and may include an overnight hospital stay. The back of the member ID card includes the member website and phone numbers to connect with customer service, speak with a nurse and discuss behavioral health. It also includes contact information for providers and pharmacists to submit insurance claims. Keep it in a safe, easily accessible place like your wallet.
Your card contains key information about your health insurance coverage that is required when you need care or pick up a prescription at the pharmacy. Keeping your card in a secure location will also help protect you from medical identity theft. The back or bottom of your health insurance card usually has contact information for the insurance company, such as a phone number, address, and website. This information is important when you need to check your benefits or get other information.
For example, you might need to call to check your benefits for a certain treatment, send a letter to your insurance company, or find information on the website. Different insurance plans sometimes cover different pharmacy networks. For example, CDPHP employer plans use a Premier network; CDPHP individual plans use a Value network; and CDPHP plans for seniors use the Medicare network. Coverage that provides for the payment of medical services as a result of sickness or injury. It includes insurance for losses from accident, medical expense, disability, or accidental death and dismemberment. The statement sent by the insurance company to the patient with a list of services provided, amount billed, and any insurance payments.
This statement normally includes any payment due from the patient, such as co-insurance, deductibles, and co-payments. The method for determining which insurance company is primarily responsible for payment when a patient is covered under more than one insurance plan. The insured's total benefits do not exceed 100% of the medical expenses.
A federal law that mandates employers with 20 or more eligible employees to provide continued health insurance under their group plan to terminated employees and their dependents. COBRA generally provides continued health insurance coverage for up to 18 or 36 months. COBRA beneficiaries may be required to pay 100 percent of the premium plus an administrative fee. A process by which the patient, their doctor, or the hospital can object to the health plan's decision not to pay for medical services.
Your BCBS ID card has your member number, and in some cases, your employer group number. Your member number, also known as your identification number, is listed directly below your name. You'll need this information when receiving medical services at the doctor or pharmacy, or when calling customer service for assistance. If your group number is available, you'll find it directly below your member number.
Approval needed for medical care beyond that offered by a primary care physician or hospital. For example, HMO plans typically require referrals from a primary care physician to see specialists. A way in which a physician agrees to accept an insurance company's payment level as payment in full. The bill is sent directly to the insurance company with payment made directly to the physician. This does not include patient's co-insurance, deductibles, and non-covered services.
Medical services received from a non-participating provider. Coverage generally requires payment of a higher deductible, co-payment, and/or coinsurance than for medical services from a participating provider. A type of cost sharing where the patient and insurance company share payment of the approved charge for covered services after payment of the deductible by the patient.
Most health care services and insurance providers have staff members specifically to help you find the information you need. The back of the member ID card may include phone numbers to connect with customer service, speak with a nurse and find behavioral health support. It also includes contact information for providers and pharmacists to submit claims. Our phones, keys, driver's licenses and credit cards are kept at our fingertips at all times. Those items are unique to each of us, and provide access to the things we need.
When it comes to healthcare services, that item is your Blue Cross Blue Shield ID card. If you have a renters insurance policy, you may need to provide proof of insurance to your landlord. Your insurance policy's declarations page will have that information and can be sent wherever you'd like. Digital insurance cards give you the ability to show proof of insurance directly on a mobile device if you are in a car accident, pulled over, registering a car, etc.
Some insurers, including Progressive, provide a digital insurance card that you can access on a smartphone or tablet via an app or by logging in to your account. Nearly every state allows you to show that electronic proof of insurance on your phone . A billing form used by hospitals to file insurance claims for medical services. A signed statement from patients or guarantors that allows physicians and hospitals to release medical information so that insurance companies can pay medical bills. A practice of some health insurance companies to deny coverage to patients for a certain time period for medical conditions that already exist when coverage began. Medicare coverage helps pay for physician services, medical supplies, and other outpatient services not paid for by Medicare Part A.
Medicare coverage that helps pay for inpatient hospital, home health, hospice, and skilled nursing facility services. The patient must pay a daily co-insurance for each lifetime reserve day used. Additionally, lifetime reserve days can only be used once during a patient's life. A type of insurance plan that provides coverage of designated health services needed by plan members for a fixed, prepaid premium.
A billing form used by doctors to file insurance claims for medical services. Integrating benefits payable under more than one health insurance . Coordinated coverage is usually arranged so the insured benefits from all sources do not exceed 100 percent of allowable ounted) medical charges. Coordinated coverage may require patients to pay some deductible or co-insurance.
Medicare coverage from day 61 to day 90 of continuous inpatient hospital stay. The patient is responsible for paying for a portion of those days. After the 90th day, the patient enters their lifetime reserve days. The portion patients must pay out-of-pocket for medical services, including co-payments, co-insurance, and deductibles.


























No comments:
Post a Comment
Note: Only a member of this blog may post a comment.